Pros and Cons of topical products containing a suspended API
Prescription drug products contain an active pharmaceutical ingredient (API)1. While traditional topical drug product development focuses on dissolving the API, challenges can arise from dissolved systems. Suspending an API can be an appropriate alternative which can lead to better drug product outcomes. The potential advantages associated with a suspension may be overlooked when developing a topical formulation.
Stability
It is not uncommon for APIs to exhibit more degradation over time in a dissolved state as opposed to a solid state. A major advantage to a suspension product is that the API can be more stable than if dissolved. This effect can be quite dramatic, as there are APIs that are not stable in a dissolved state and must therefore be suspended (e.g. Bacitracin Ointment). Using this advantage for marginally stable dissolved products can have significantly stabilizing effects.
Cosmetic Elegance
Being hamstrung to formulate with specific solvents (at adequate concentrations) to ensure API dissolution can be difficult and limit dosage form options. Without the need for a dissolving solvent system, a more cosmetically elegant formulation can be made that may lead to better patient compliance.
Targeted Delivery
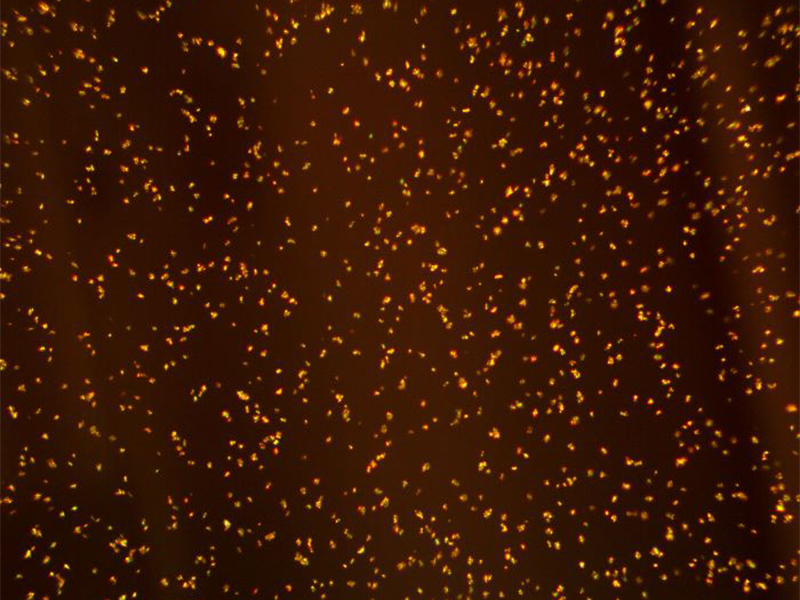
Micronizing an API to a size of < 10 microns is critical for suspended products and, fortunately, technology and resources for micronizing to this size are readily available. API particles < 10 microns can penetrate the outer layers of the stratum corneum2 and hair follicles of intact human skin. Normal cracks and breaks in the stratum corneum can be as large as 100 microns3, facial pores can range from 250 to 500 microns in size4, and the size of a hair follicle is 65 to 100 microns. Given these dimensions, one can see how small, suspended particles can enter into the skin layers intact.
Depot Delivery
When a micronized API particle does work its way into the stratum corneum, a hair follicle, or a pore, it will typically have to dissolve in order to further penetrate to have activity at the site of action. While this dissolution can be slow due to poor solubility within the skin, the dissolution does still occur. Rarely are solubilities on or in the skin truly zero. This effect could have an additional benefit of the solid drug particle acting as a depot, supplying a constant source of slowly dissolving API into and through the skin layers.
Regulatory Considerations
While increased API stability, the ability to make cosmetically elegant formulations, and the ability to depot the API into the skin provide advantages in some situations, there are regulatory requirements to consider with suspensions. Specifically, FDA will require proof that the size, amount, and crystal habit of the API particles do not change over time. The methodology for performing these tests has been established with laser diffraction, particle sizing, and x-ray crystallography. Additionally, it is necessary to ensure the particles are uniformly suspended during manufacture and remain so throughout the product shelf life.
References:
- “Drugs @ FDA Glossary of Terms.” November 2017. FDA/Center for Drug Evaluation and Research, Office of Pharmaceutical Quality, Office of Policy for Pharmaceutical Quality.
- M. Schneider, F. Stracke, S. Hansen, and U.F. Schaefer. “Nanoparticles and their interactions with the dermal barrier,” Dermato-endocrinol. 2009 Jul-Aug; 1(4): 197–206. doi: 10.4161/derm.1.4.9501
- A.K. Dąbrowska, C. Adlhart, F. Spano, G. Rotaru, S. Derler, L. Zhai, N.D. Spencer, and R.M. Rossi. “In vivo confirmation of hydration-induced changes in human-skin thickness, roughness and interaction with the environment” Bio-interphases. September 2016 11(3):031015 doi:10.1116/1.4962547
- F. Flament, G. Francois, H. Qiu, C. Ye, T. Hanaya, D. Batisse, S. Cointereau-Chardon, M.D.G. Seixas, S.E.D. Belo, and R. Bazin. “Facial skin pores: A multiethnic study” Clinical, Cosmetic and Investigational Dermatology. February 2015. doi: 10.2147/CCID.S74401